As USA faces cancer drug shortage… Cancer Society in 2020 fretted over 'carbon footprint of cancer care' –
AND –
Politco June 2023: Hospitals Turning into ‘Climate Change Fighting Machines’ – ‘More Earth-friendly drugs’ – Reducing ‘anesthetic gas’https://t.co/xwz1EYSLDS https://t.co/DLPBjXdJYJ pic.twitter.com/hUAzDWRx6g
— Marc Morano (@ClimateDepot) June 19, 2023
https://www.politico.com/news/magazine/2023/06/06/hospital-climate-change-waste-00098612
By JOANNE KENEN
Inside the greening of American health care.
Excerpts: Sometimes they’ll use more Earth-friendly drugs when appropriate. They’ve already stopped using another common anesthetic gas, called desflurane, which remains in the atmosphere for a decade or more, according to Shira Abeles, an infectious disease physician at UCSD, who recently became its medical director of sustainability.
She’s got plenty of science backing these shifts. The American Society of Anesthesiologists has identified alternatives that are better for the planet, just as safe for patients — and often cheaper.
“One hour of that volatile agent (desflurane) is equivalent to driving a car 250 miles, a gasoline car, I should say. And there’s very little we do in one hour,” said Joanne Donnelly, who, as director of the nurse anesthesia program at the University of Minnesota, has trained personnel in sustainable practices in hospitals across Minnesota and Wisconsin.
“Extrapolate that across an urban area, a region, a nation,” she said. “It’s an incredible impact.”
The drive to reimagine anesthesia is part of a broader if belated effort to decarbonize U.S. health care, from the operating room to the cafeteria to the gardens and grounds. It’s a push spurred on by both medical professionals and Washington policymakers, who feel increased pressure to act amid the dangers of climate change and who acknowledge health care has been slow to engage on sustainability.
The health sector is responsible for 8.5 percent of U.S. emissions of greenhouse gases including carbon dioxide, methane and ozone — an outsized impact compared to the rest of the world. (Globally, health care systems contribute roughly 4.6 percent of total greenhouse gas emissions.) Without huge new efforts, the U.S. will have trouble reaching its ambitious emissions reduction goals.
Within American health care, hospitals are the biggest source of emissions, not to mention generators of enormous amounts of nonrecyclable trash from all the single-use, disposable devices and supplies that head swiftly into landfills and incinerators.
Not every hospital is on board with transformation. Change can be expensive, and it’s always hard to overcome the inertia of the status quo. But health leaders see progress, and the Biden administration is doing its own part to push hospitals to overhaul their practices — with some success. The question is, will it be enough?
…
Hospitals in Vermont and Boston are growing vegetables in rooftop gardens; Seattle Children’s Hospital is planting conifers in greenery-starved poor neighborhoods. In drought-prone Los Angeles, a UCLA plastic surgeon suggested timers for operating room sinks; everyone still scrubs in, of course, but without wasting water.
Some hospitals offer more plant-based meal options; New York Mayor Eric Adams, who follows a mostly vegan diet, saw to that in the city’s 11 public hospitals.
Meanwhile, recycling medical waste is neither easy nor inexpensive; it’s more complicated than tossing a tuna can or yesterday’s newspaper into a blue bin. But that’s slowly changing as more health systems turn to FDA-certified companies that can recycle, sanitize or reprocess such waste.
…
It’s become harder to ignore how extreme climate events and pollution endanger human health, with poor people, minority groups and elderly people particularly vulnerable. Extreme weather exacerbates heart, lung and kidney disease; it makes asthma worse. Mental health deteriorates. Heat waves kill people — directly, or by aggravating chronic conditions. Power outages in patient homes mean no refrigeration for insulin or electricity to keep oxygen tanks flowing.
…
“What excites me is that health professionals are starting to connect the reason why they’re there in the first place, which is to take care of patients, with the health impacts that are happening because of climate [which] their health systems are contributing to,” said Shanda Demorest, a nurse who is associate director for climate engagement and education at Health Care Without Harm, which along with its Practice Greenhealth arm, is a major force in pushing for new health and climate work.
The Veterans Administration and the Indian Health Service, which deliver health care to millions of people across the country, have been directed to reduce emissions and energy use as part of the Biden White House’s overall government climate policy.
For the rest of the health care system, HHS unveiled a Climate Pledge on Earth Day 2022 to spur more action. … About 116 health organizations, representing 872 hospitals as well as other health care sectors, have signed on. Along with the federal health systems, that represents about 15 percent of U.S. hospitals, HHS officials said.
…
The climate pledge is voluntary, but hospital sustainability experts insist it’s not the usual feel-good exercise. Signatories commit to specific actions and must publicly report progress toward cutting emissions by 50 percent by 2030 and cutting net emissions by 100 percent by 2050.
…
If hospital leaders start to perceive climate action as unavoidable — either because they anticipate it will be mandated or because they will face mounting pressure from within, particularly from younger doctors and nurses — they may start sooner rather than later.
HHS is aware that not all health systems are committed, and that even those that are may need help. McCannon said HHS is rolling out technical assistance and some grants.
…
But activists and sustainability teams want more. More tools. More metrics. More financial help.
…
Some advocates would like to see the federal government impose tough regulations and requirements to force change. Others suggest building incentives into Medicare payments to hospitals, which would give a government-imprimatur on health care greening without creating a new mandate. Climate benchmarks could be included in HHS’ “conditions for participation,” the practices that health providers must follow to be eligible for Medicare or Medicaid payments.
#
Related:
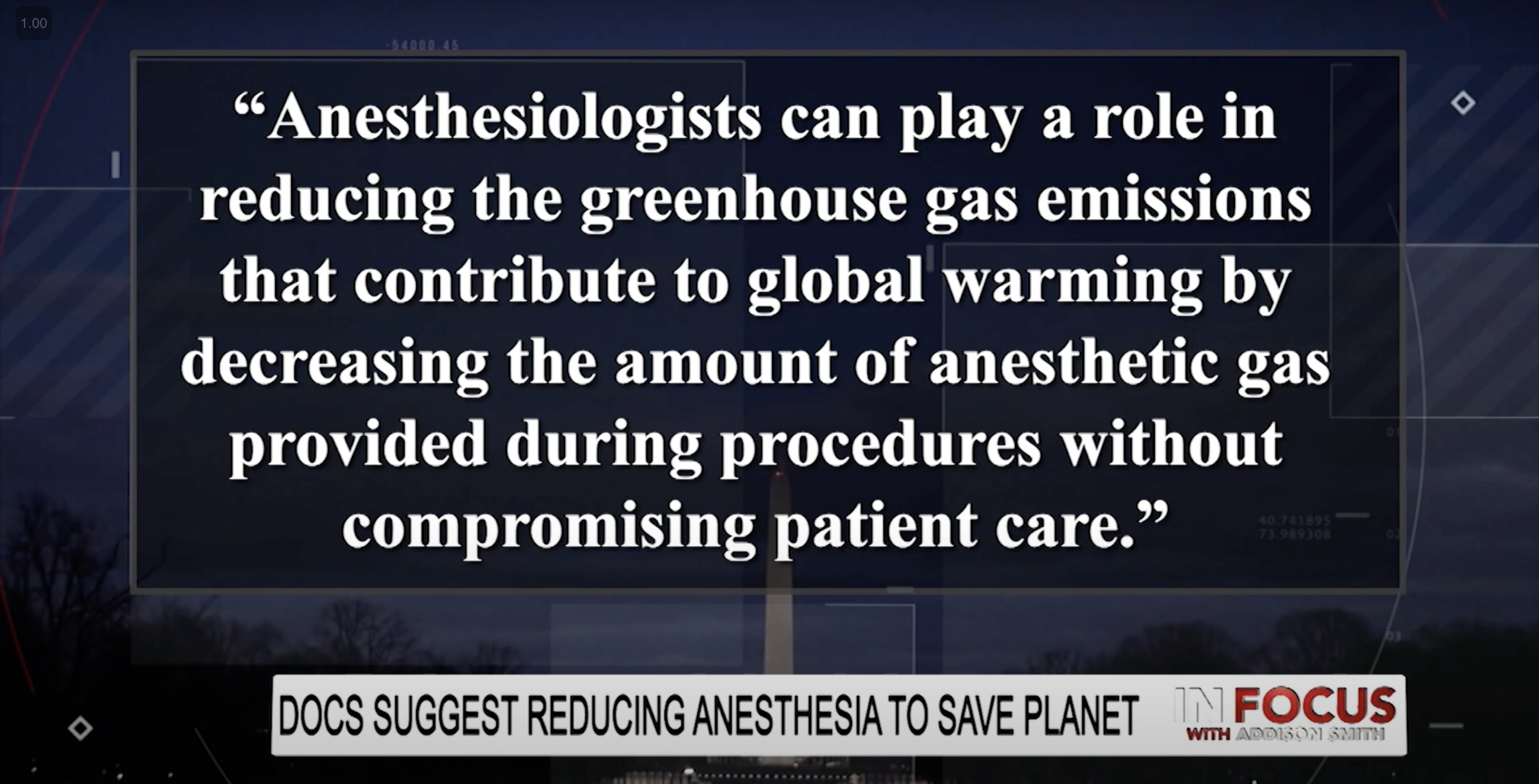
Anesthesia the next target in climate battle: Docs suggest reducing anesthesia: Would you suffer to combat climate change?
NY Post: Dr. Mohamed Fayed, a senior anesthetist at Detroit’s Henry Ford Health, made the suggestion during the American Society of Anesthesiologists’ annual conference last Friday in Orlando, Florida. “Global warming is affecting our daily life more and more, and the reduction of greenhouse gas emissions has become crucial,” he said. Dr. Fayed added, “No matter how small each effect is, it will add up. As anesthesiologists, we can contribute significantly to this cause by making little changes in our daily practice — such as lowering the flow of anesthetic gas — without affecting patient care.”
Study press release:“Anesthesiologists can play a role in reducing the greenhouse gas emissions that contribute to global warming by decreasing the amount of anesthetic gas provided during procedures without compromising patient care, suggests new research being presented at the American Society of Anesthesiologists’ ADVANCE 2023, the Anesthesiology Business Event.” [Climate Depot Note: The American Society of Anesthesiologists’ website appears to have pulled the article. but it is available here. & here.]
Research notes that inhaled anesthesia accounts for up to 0.1% of the world’s carbon emissions, which are regarded as the primary driver of global climate change. An hour of surgery using an inhaled anesthetic is equivalent to driving as many as 470 miles, according to a 2010 study.
#
Flashback 2020 Study in American Cancer Society Journal in 2020 Fretted over ‘carbon footprint of cancer care’ – ACS Journal: “Climate change and cancer” – Excerpt: “To date, no studies have estimated the carbon footprint of cancer care…The energy expenditure associated with operating cancer treatment facilities and medical devices, as well as the manufacturing, packaging, and shipment of devices and pharmaceuticals, contributes significantly to greenhouse gas emissions in cancer care…Some cancer treatment facilities have begun to consider their own carbon footprint and started a process to achieve carbon neutrality.”
Climate Depot’s Morano: “Here is a question for the American Cancer Society: If you need cancer treatment, would you go to a cancer treatment center that was worried about its carbon footprint? Or one that was worried about delivering the best possible modern care possible?”
#
How many can they come up with? Surgery Causes Global Warming?! Study Shows ‘Anesthesia Agent Is Greatest Potential Contributor to Global Warming’ – Claim: ‘Anesthetics used by a busy hospital contribute as much to global warming as the emissions from hundreds of cars per year’
Restrict anesthesia to save climate & Harvard Med to ‘Integrate Climate’ Into M.D. Curriculum & American Cancer Society Frets ‘carbon footprint of cancer care’ – The Great Medical Reset: Your Doctor will treat the climate first — not your well-being — and you will be happy. Doctors care more about planetary care than patient care.
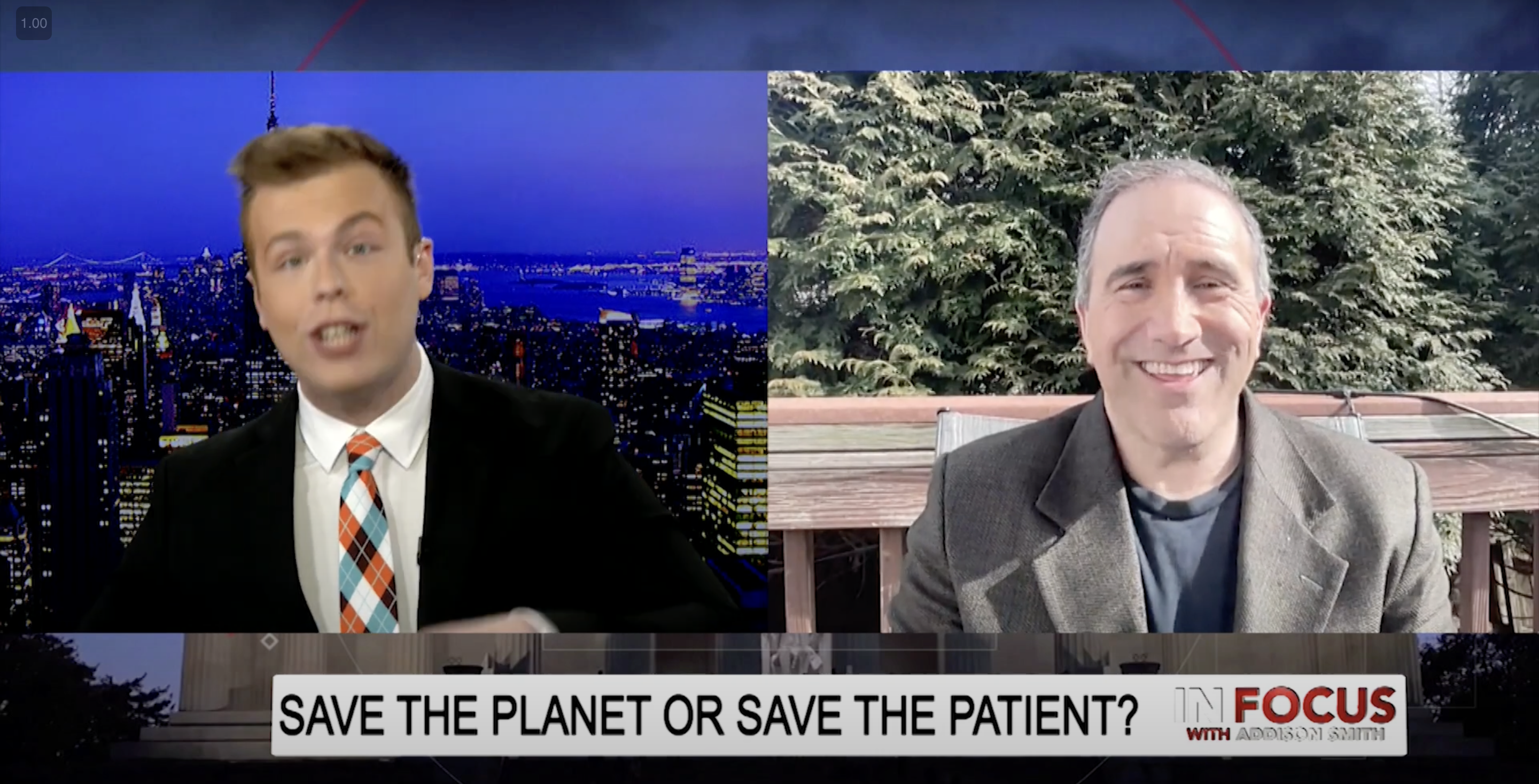
Climate Depot’s Marc Morano on Addison Smith’s In Focus on One America TV – Broadcast Feb. 8, 2022.
 .
. 
 .
. 
Reuters: Cannabis users may need ‘more than TWICE usual dose’ of anesthesia for surgery – “People who regularly use cannabis may need more than twice the usual dose of anesthesia for surgery, a U.S. study suggests.”
Claim: Surgical General Anesthetic is Contributing to Climate Change– Switching from general to regional anaesthetics may help cut greenhouse emissions and ultimately help reduce global warming, a new study claims. While regional anaesthetics numb a certain part of the body, general anaesthetics make patients totally unconscious for what tend to be more serious procedures. But unlike regional anaesthetics, generals use volatile and environmentally-unfriendly halogenated agents, such as desflurane, or nitrous oxide. … ‘Green-gional’ anesthesia: the non-polluting benefits of regional anesthesia to decrease greenhouse gases and attenuate climate change
#How many can they come up with? Surgery Causes Global Warming?! Study Shows ‘Anesthesia Agent Is Greatest Potential Contributor to Global Warming’– Claim: ‘Anesthetics used by a busy hospital contribute as much to global warming as the emissions from hundreds of cars per year’-
Claim: Surgical General Anesthetic is Contributing to Climate Change– Switching from general to regional anaesthetics may help cut greenhouse emissions and ultimately help reduce global warming, a new study claims. While regional anaesthetics numb a certain part of the body, general anaesthetics make patients totally unconscious for what tend to be more serious procedures. But unlike regional anaesthetics, generals use volatile and environmentally-unfriendly halogenated agents, such as desflurane, or nitrous oxide. … ‘Green-gional’ anesthesia: the non-polluting benefits of regional anesthesia to decrease greenhouse gases and attenuate climate change
Flashback 2019: Canadian Medical Association Journal: How health care contributes to climate change – Climate change is a growing health threat around the world — contributing to heat stroke, food insecurity, cardiorespiratory ailments and many other issues — and the health care industry is part of the problem. “It’s almost like the process of healing causes harm,” said Kent Waddington, cofounder of the Canadian Coalition for Green Health Care. Health care in Canada was responsible for 4.6% of national greenhouse gas emissions in 2009–2015, according to a recent study in PLOS Medicine. … The Canadian Coalition for Green Health Care has led projects to reduce the environmental impact of providing health care, such as promoting sustainable food in hospitals and reducing toxic chemicals used for cleaning.
2022: Operating rooms are the climate change contributor no one’s talking about – Two surgeons-in-training suggest some sustainable solutions for their energy-intensive discipline. ... Cancer care is an obvious target for greener efforts within surgery, Berlin notes, because it often involves intense levels of care over a short period of time. Plus, minimally invasive surgeries that require a lot of energy, including robotic-assisted operations, have become common treatments for cancers ranging from colorectal and uterine cancer to head and neck cancer. A robotic-assisted hysterectomy, for example, produces as much carbon as driving more than 2,200 miles in a car — the equivalent of a road trip from Ann Arbor, Mich., to Los Angeles. … Cancer care is an obvious target for greener efforts within surgery, Berlin notes, because it often involves intense levels of care over a short period of time. But perhaps the broadest way the oncology space could cut down on its greenhouse gas emissions is to change how surgical care is delivered, starting with permanently offering telemedicine.
2022: Association of American Medical Colleges: Hospitals take creative steps to reduce carbon footprint – As medical organizations increase their commitments to reduce greenhouse gases, hospitals report progress through quiet methods like changing anesthesia, fixing valves, and re-sterilizing devices.
Linnea Lueken: “Recommends that hospital staff mitigate this alleged danger, primarily by using less anesthesia, or opting for the use of less effective topical or more dangerous intravenous methods because “they have less of a negative environmental impact.” …. Doctors don’t use anesthesia for fun, they do it to reduce pain during medical procedures. These misanthropic M.D.s are advocating nothing more nor less than allowing people to suffer in the name of sustainability. …
We have protocols in place to limit medical tests on human subjects without their consent. Hospitals should be devoted to healing patients, not experimenting in loony sustainability projects on captive subjects.”